I’ve now had time to read the Social Democrat’s health policy in their manifesto. Their overall goal is to create an Irish NHS, a single tier, comprehensive health care system, largely free at the point of use. This is a sensible, clearly described goal, which would improve health care in Ireland. The British NHS is not perfect, but it is a lot better than the Irish system, and a lot cheaper too. This forms part of their strategy to reduce the costs of living in Ireland.
There are three sections, one on acute healthcare, one on mental health, and one on disability services. Health care for older people is discussed as part of a broader section on support for older people.
The acute services section is labelled ‘BUILD AN IRISH NHS’. Ironically most of the text talks about hospitals, trolley waits, ambulances, waiting lists for surgery, travel for procedures. There is a stated aim to have a community care focus in the system, but it is not clear what this would mean. The practical measures listed include supporting staff, by, for example, encouraging the recruitment of GP’s and nurses, building more primary care centres; improving access by, among others, formal resource allocation methods, wider access to free GP care, aggressive health promotion, reducing administrative costs, and aligning hospital group borders and community health office borders; improve service delivery by setting up minor injury units, improved access to diagnostics technology both for A/E and for GP’s, and getting 5 chronic disease management programs running.
They also say ‘Implementation is as important as policy in health reform’ , with which I agree strongly! To support implementation, they will set up a long-term vision for health care, with staff and patients; work across all of government; make health service data more open, and remove perverse incentives. They also suggest reducing prescription charges for GMS users, in the first section of the manifesto.
All of this is laudable, and some of it may well be achievable. The idea of settling on a clear vision for the service is appealing, although more detail about how this is to be done would be welcome. It is still too hospital focused, and I do not think they quite get the scale of the resources required to resource general practice properly. There isn’t a clear commitment to free GP care, nor to the level of resources in general practice needed for this. Reducing administrative costs sells well to the public, but would probably prevent any effective change. As I never tire of saying the health services have too many administrators, but not nearly enough managers.
Under the heading ‘EMPOWER THOSE WITH DISABILITIES’ there is a strong and positive discussion of the issues for people with disabilities. The core of their policy is to ratify the UN Convention on the Rights of Persons with Disabilities, which would be very welcome. Other policies include supporting people with disabilities in living independently, in finding and keeping work, and in staying out of poverty. They don’t discuss the individualization of payments, where the disabled person, and not the service supporting them, gets state funding, and their vision does not really cover problems like high rates of imprisonment for people with intellectual disability, but the remainder would be a welcome new focus on disability care.
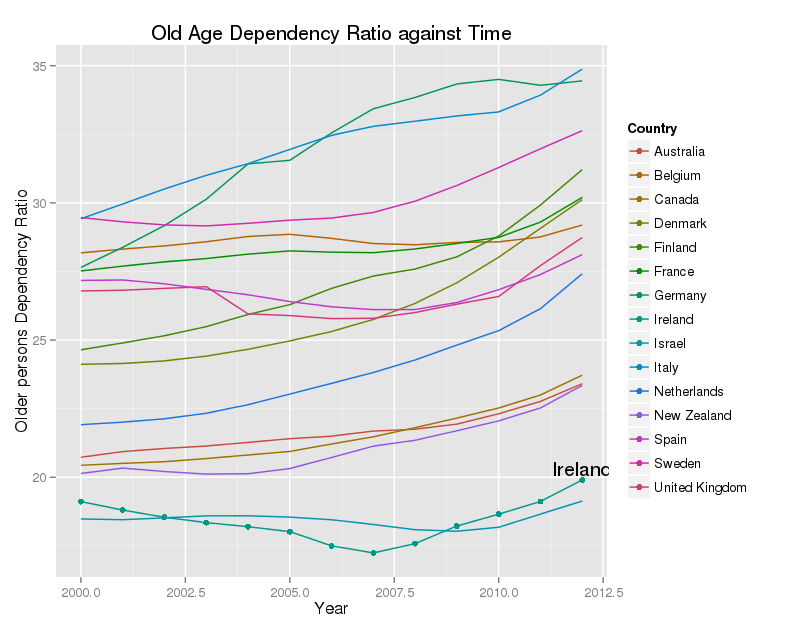
For older people, they suggest expanding the Fair Deal scheme to over home care packages, increasing access to medical cards for older people, and improving the benefits to carers of their PRSI contributions. Reducing prescription charge would also benefit older people significantly.
Under ‘SUPPORT MENTAL HEALTH’ they call for full implementation and resourcing of Vision for Change, the (very good) 2006 mental health strategy. They will expand services to detect difficulties in infancy, and to improve the mental health of school children. They will increase resources for suicide prevention, and support the much wider use of non-drug therapies for mental health problems. Additional ring-fenced resources will be set up for some high risk or marginalised groups, including young parents, Travellers, and asylum seekers. They will require a much greater emphasis on effective care for people with a ‘dual diagnosis’ – addiction and a specific mental health problem.
Overall, this is a reasonable policy. It’s not clear how much it would cost, which is a huge omission, but I think a process starting with developing a common vision for services, and with a focus on community care, might get us somewhere. At least implementation is discussed, which is unusual in political manifestos. There is no discussion of the need to fix the culture of HSE, nor of the need to improve accountability. There is not enough thought given to general practice, a blind spot shared with the Department of Health. Some of the proposals would not work – notably reducing health service administration, and aligning community health services to hospital group boundaries. However, all in all, this is a policy with many positive features.